Sleep Apnea
Understanding the Basics of Obstructive Sleep Apnea
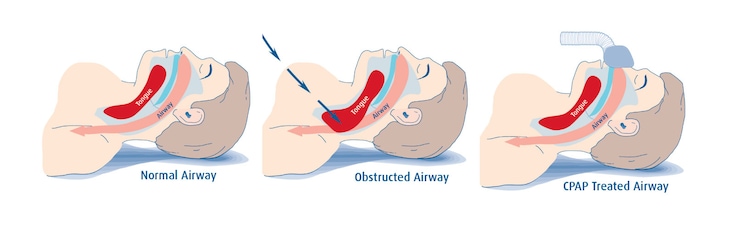
With obstructive sleep apnea (OSA), your breathing airway partially or completely collapses during the deep or rapid eye movement (REM) sleep stages when we are meant to physically and mentally recuperate from our awake time during the day. As the airway softens, getting smaller in size, the resistance to airflow leads to an increase in your work of breathing. This may progress further to a complete collapse of the airway, holding your breath long enough to see a drop in your blood oxygen levels. Your body will respond with an adrenaline or “panic” arousal that returns you to the non-restorative light sleep stage, or may even cause you to wake up during the night.
Approximately 30% of Canadians are at a high risk of developing sleep apnea. Men are two times more likely to report being diagnosed compared to women. This may be due women presenting differently from men. Common symptoms include excessive daytime sleepiness and fatigue, snoring, morning headaches, high blood pressure, mood changes with irritability, and leg cramps. Untreated OSA can lead to a higher risk for heart failure, stroke and diabetes.
How is it diagnosed?
If you suspect that you may have OSA, speak with your family physician who may refer you to a physician who specializes in sleep disorders. There are two frequently used tests to diagnose OSA. The first is an overnight sleep study called a polysomnogram. This test is done in a sleep laboratory where it records activity of the brain, leg, arm and chin muscles, eye movement, nasal and oral airflow, respiratory effort, snoring and oxygen saturation. The second test is called a Home Sleep Apnea Test or HSAT. As you can tell by the name, this test is done at home and measures nasal flow, snoring, respiratory effort, oxygen saturation and sleep position.
How is it treated?
While CPAP is the preferred therapy, for some individuals with mild to low-moderate OSA, an oral appliance may be an alternative. These devices are customized to your mouth and made by dentists trained in dental sleep medicine appliances. Conservative therapy includes alcohol avoidance, sleeping in a side position, use of a nasal decongestant and weight loss. Surgery is an invasive intervention that may reduce snoring but may be less helpful for OSA. Your physician will decide on the best treatment plan for you.